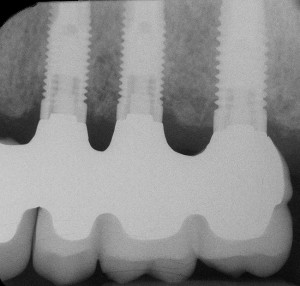
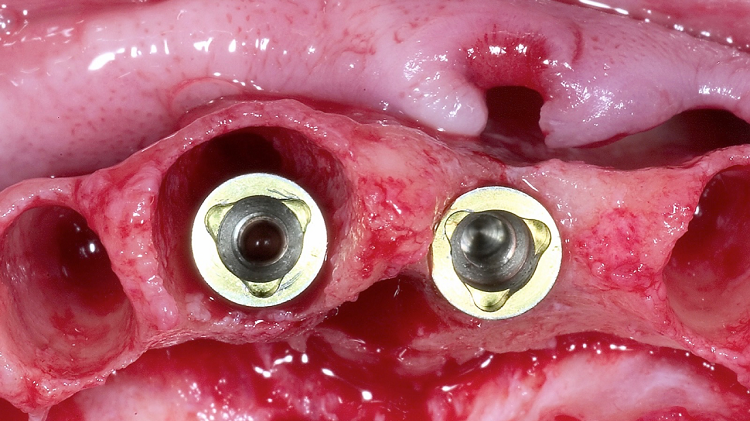
Many of you may have encountered a clinical outcome similar to the above image. This is definitely a result we never want to see, but in the world of immediate dental implants there remains a certain amount of uncertainty about what an implant and its surrounding gingival tissues are going to look like in 10 years.
In 1998 or thereabouts researchers were giving opinions on when an implant surgeon did and didn’t have to combine bone grafting with an immediate implant.
Even in my own residency some of these notions from that time period were still hanging around.
I recently was fortunate enough to listen to an interesting lecture by Dr. Joseph Kan. Dr. Kan is a prosthodontist in practice in California. He also happens to teach at Loma Linda School of Dentistry. During his lecture he showed multiple cases of anterior immediate dental implant outcomes. He categorized the cases into the following:
-Immediate implant with no bone grafting
-Immediate implant with bone grafting in the remaining socket space (the gap)
-Immediate implant with bone grafting in the remaining socket space, and bone grafting placed on the facial aspect of the intact buccal plate.
His results were impressive. He was able to demonstrate that immediate implants placed without any grafting tended to show significant facial bone resorption and recession of facial gingival tissues which started to show up around 8-10 years post-operatively. (Dr. Kan reported his plans to publish his findings in the Journal of Oral & Maxillofacial Implants.)
His categories evolved with time so he has fewer cases and less data on immediate dental implants with bone grafting in the gap and even less on immediate dental implants with bone grafting in the gap and on the facial bony wall, but even with fewer data, he made a compelling case:
Immediate dental implants will likely have much more predictable bony and soft tissue outcomes in the long run if bone grafting is done both in the remaining socket space (regardless of the gap size), and on the facial aspect of the bony wall (outside the socket walls).
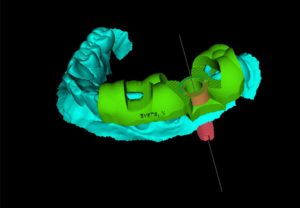
My own bone graft protocols are as follows:
-Autogenous and/or allograft bone placed in all remaining socket spaces in all immediate implants
-bovine derived xenograft placed outside the socket walls to augment and give long term support to the facial gingival tissues.
What have you had success with?