I remember when I started placing implants feeling really confused about all the different types of connections among not only implant brands, but implant lines within individual brands.
There was an ‘external hex’ and an ‘internal hex’. Then there was a ‘trilobe’ and even an ‘octagon’.
‘Internal Conical Connection’ began to be something I heard more often, but even then there were brands making noise about a hex on top of a ’12 point dual hex’ or a ‘synocta connection’. Connections were ‘certain’ and who is “Morse” and why is his Taper so fascinating?
Well it turns out there is some important science to what type of connection you are using. Specifically it appears to have some profound effects on crestal bone levels and even incidences of peri-implantitis.
I should say that with all of these concepts we encounter in implantology, whether it be ‘platform switching’, ‘bone-level vs tissue-level’, ‘butt-joint connections vs conical connections’, you cannot make one of them your pet and devout all your time and attention to it and leave out all the other important aspects. They all need to be considered and weighed together as you make your clinical decisions.
Connections are important though and the reasons we like a true internal conical connection is as follows:
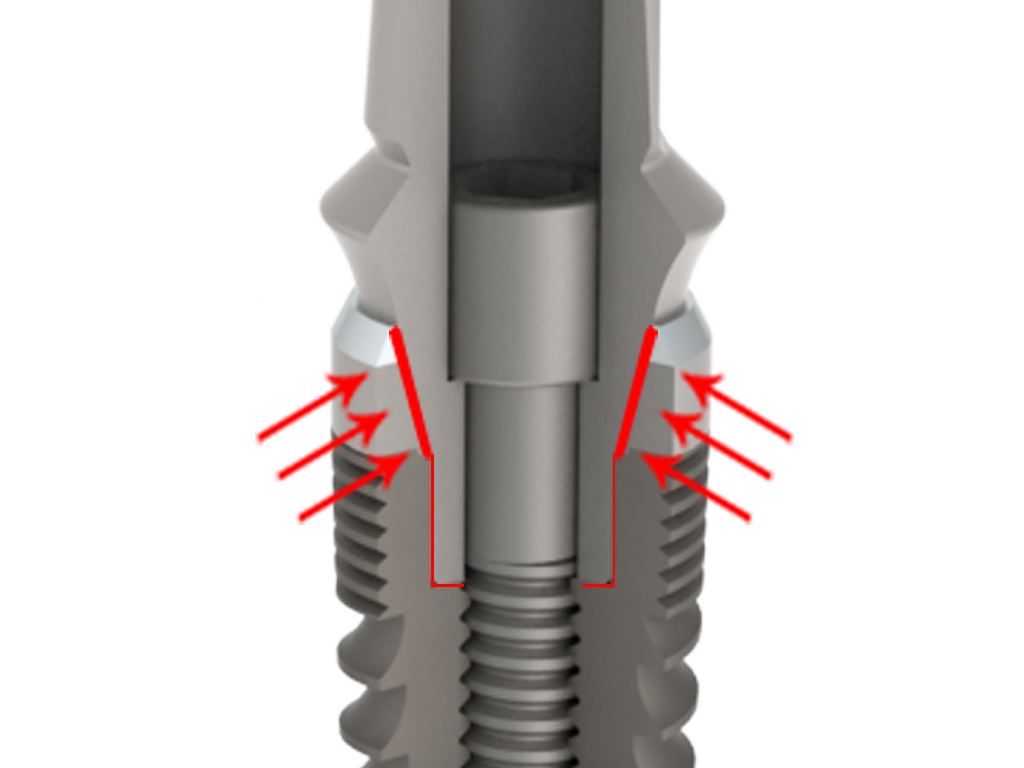
- Research seems to support that internal conical connections are less prone to exhibit a micro-gap between the implant and abutment. This is not so in other connection types. A severe micro-gap may explain one mechanism why implants develop peri-implantitis and bone loss leading to esthetic failure and possibly total implant failure.
- A conical connection appears to cause a true ‘hermetic seal’ on the implant abutment interface. I liken this property to creating a good seal on a root canal. You don’t want to give bacteria a home within a root canal treated tooth, nor do you want to with an implant.
- A conical connection appears to keep the implant and abutment joined as one without differential movement. Meaning that as a patient chews on their restored implant over and over there is less abrasion between the abutment and implant and there is less loosening of the abutment from the implant because the two move and respond to forces as a single unit.
An excellent video worth watching on all of these key points is a youtube video showing research done by Dr. Zipprich.
Enjoy!